What is Obsessive Compulsive Behavior Disorder?
Obsessive Compulsive Behavior Disorder, also known as OCBD, is a condition often overshadowed by its more widely known relative, Obsessive Compulsive Disorder (OCD). While they share similarities, it is critical I point out that OCBD stands distinct with its unique characteristics and challenges.
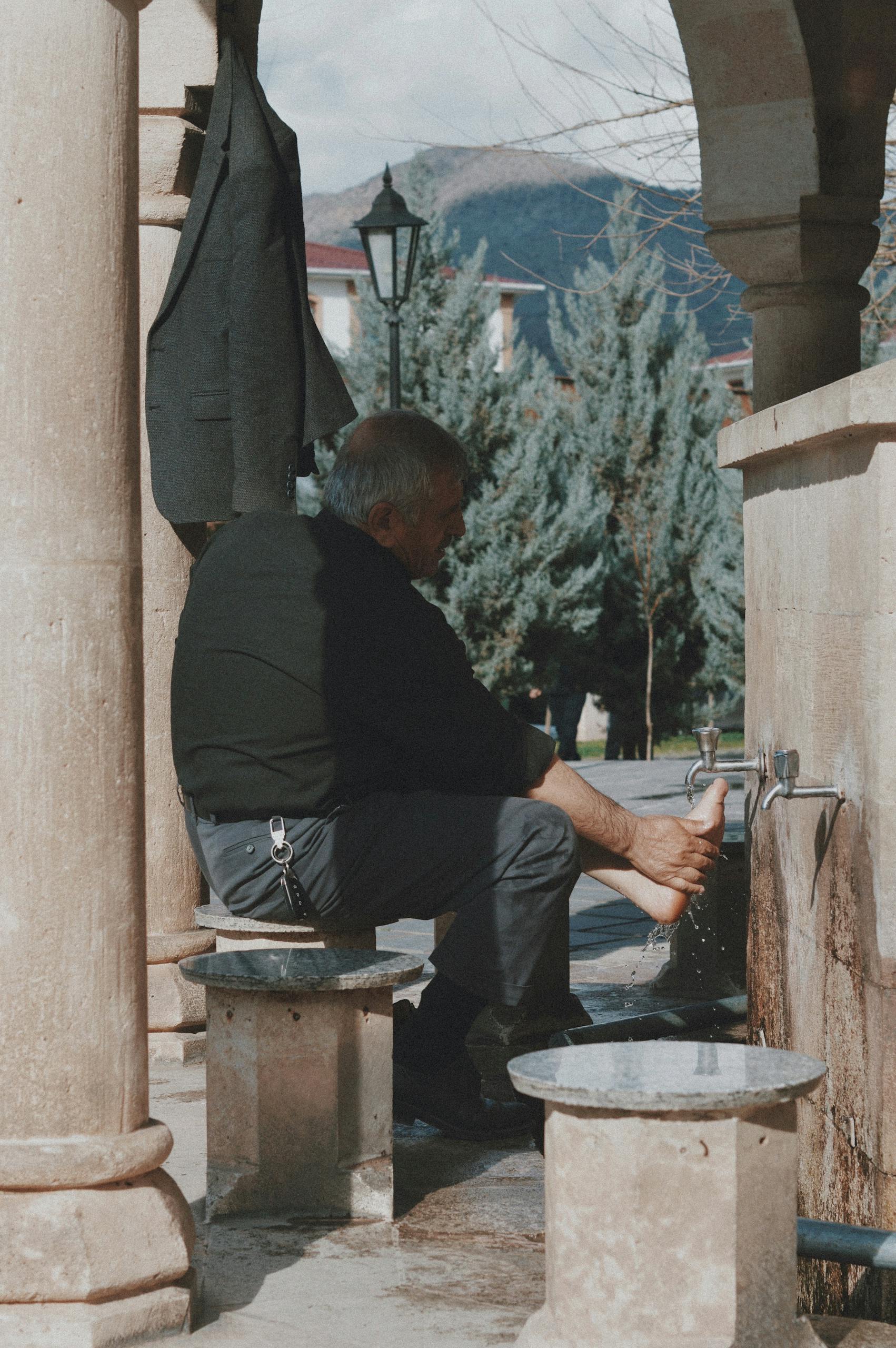
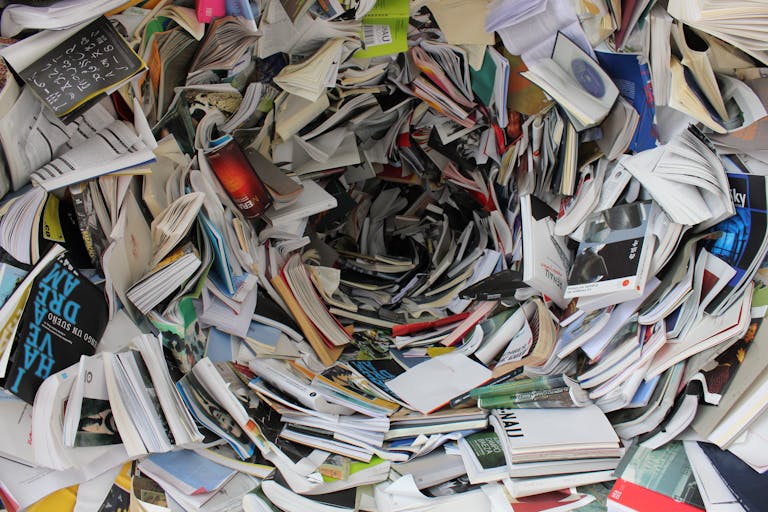
If I were to outline what makes OCBD stand out, it is the persistent, repetitive behaviors or mental acts that individuals feel driven to perform, even though they may recognize them as unnecessary or irrational. Think of it as a loop of unwanted behavior that a person feels they cannot simply shut off.
Early recognition of OCBD is vital. Why? Because the longer it goes unaddressed, the more ingrained these behaviors can become, making treatment and management much harder later on. I am talking about issues ranging from disrupted daily routines to strained relationships.
Now, one problem I see all too often is the whirlpool of common misconceptions. I get it; it is easy to chalk up certain repetitive behaviors to just ‘being a little OCD,’ but that oversimplification can prevent people with OCBD from seeking the help they actually need.
Exploring the Underlying Causes of OCBD
Unraveling the causes of Obsessive Compulsive Behavior Disorder (OCBD) is not straight forward. Unlike a common cold, where you know exactly what brings about the sneezing, OCBD is complex, with a myriad of factors at play. I will guide you through the major influences that researchers have identified, each shining a new light on this condition.
Genes may play a role. Just as you inherit your eye color from your parents, there is evidence to suggest that OCBD could be passed down through families. Studies have shown that if a close relative has OCBD, your risk of developing the disorder may increase. This does not mean fate is sealed by your DNA, but it is a piece to consider in the larger puzzle.
Your environment could be a trigger. What you have lived through matters. Traumatic events or high-stress situations might set the stage for OCBD to emerge. Drawing a line between cause and effect here is challenging, but understanding the impact of life experiences provides a valuable context for the disorder.
Then there is the brain itself. It is the command center, responsible for every thought, action, and feeling. In people with OCBD, certain areas of the brain might work differently. This is not to say they are faulty; rather, it highlights unique patterns that could contribute to the behaviors we see in OCBD.
Finally, stress and trauma cannot be ignored. While not every stressful event will lead to OCBD, for some individuals, it could be the tipping point. It can be the stress that accumulates over time or a traumatic incident that flips the switch, underscoring the need for strategies to manage adversity.
OCBD in Relation to Other Disorders
It is important to see OCBD not as an isolated ailment, but as a condition that frequently intersects with other disorders. The link between OCBD and its better-known relative, Obsessive Compulsive Disorder (OCD), is particularly significant. While they share some similarities, the presence of distinct behavioral patterns in OCBD differentiates it from OCD.
A deeper look into OCBD often reveals a tapestry of anxiety disorders. It is not uncommon for people with OCBD to experience general anxiety, panic disorders, or phobias. The overlapping symptoms can complicate diagnosis and treatment, highlighting the need for careful evaluation.
Comparing OCBD to other behavioral disorders, like addiction or impulse control disorders, is crucial. Although behaviors in OCBD may appear repetitive, they are not typically driven by addiction or impulse. Instead, they are performed in response to an obsessive thought or concern.
The profound impact of OCBD on a person’s day-to-day life cannot be overstated. From routine activities to work and relationships, the disruption is far-reaching. It affects mental health, fostering feelings of distress, embarrassment, or even self-loathing in severe cases.
Acknowledging these challenges, treatment often involves a combination of therapy, medication, and support networks. Cognitive Behavioral Therapy (CBT) has shown effectiveness in managing symptoms. Medications, such as SSRIs, may also provide relief. Equally important is the role of support—a network of healthcare providers, peers, and family—cultivating an environment conducive to recovery.
In conclusion, understanding OCBD’s place within the broader spectrum of mental health disorders is crucial for developing effective treatment plans. While it is a complex and often misunderstood condition, advancement in therapeutic strategies continues to improve lives. If you suspect you or someone you know is dealing with OCBD, I encourage you to reach out for professional help. An accurate diagnosis is the first step toward regaining control and enhancing quality of life.